If I had a pound every time a patient says spinach is high in iron in the clinic, I reckon I would be relatively wealthy. Also, if I knew what I was about to find out about this story whilst researching it, I would have looked into this much earlier. Thanks to Andy Brunning at compoundchem.com for the story background and links, a story of the importance of evidence and good referencing.
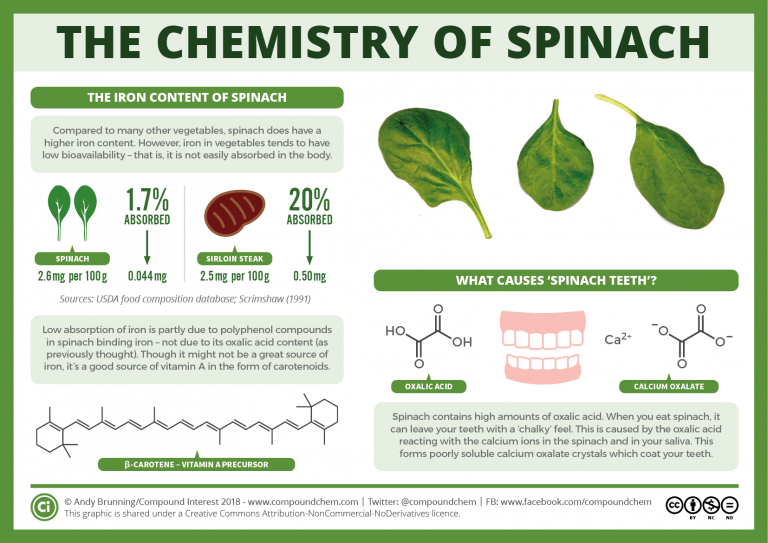
Although spinach is a green vegetable, which is particularly versatile and useful to include in a healthy balanced diet, the above infographic from Compound Chem shows the availability of iron from spinach is poor, unfortunately. So, what does it contain that is great for nutrition? Spinach is a good source of manganese, folate, vitamin A, vitamin K and fibre, which is excellent, as the fibre at least is an essential part of the diet if you are following a low fodmap diet. It is the content of polyphenols in spinach that bind with the iron rendering it insoluble, not the fact that it is a non-heam source, which is usually able to be absorbed, if a source of vitamin C is consumed at the same time.
The type of polyphenol compounds found in spinach varies but the example below accounts for the majority of polyphenol compound at 37.37 mg/100g FW. What no-one seems to have considered here is what effect microbial interaction in the bowel has on these polyphenols. Whether microbial digestion of these polyphenols affects their structure and whether this process helps the availability of iron to digestion. Interesting, Huh? Needs investigating – Yes!

Many people assuming that spinach is high in iron is probably due in part to social history. Popeye, a cartoon character developed in 1931, ate spinach to give himself ‘strength’ – “I’m strong to the finish cause I eats mi spinach”. But an original report of the iron content of spinach was stated to have contained a decimal point error, that gave the iron content as 10 times more than the actual amount. This is what I was told, as a student from 2003-2007, although others report that this was an error of reporting the iron content of dried spinach as fresh spinach. But whatever the cause, the erroneous reporting of the content of iron from spinach being higher exists to this day and has consequences. This is a particularly pervasive nutritional myth that has been investigated and reviewed by Sutton and published in the Internet Journal of Criminology, see the link below, it is a fasinating read of failings to attribute data with references and looking for clues from original sources.

Spinach does have the same iron content as some meat, but the important point to note is the availability of the iron from both foods. Spinach is a poor source, and as I have stated before in this blog, micronutrients need to be absorbed for them to be useful to us, it is no good just looking at the bare numbers. Also, Sutton states it was, in fact, the vitamin A content that Popeye was eating spinach for. This may be true, as spinach is a good source of vitamin A, from carotenoids. But also reminds me of another UK wartime ‘fable’ of eating plenty of carrots to improve eyesight. Improved eyesight only occurs if someone has a severe vitamin A deficit and night blindness, no improvement is gained with those who have adequate vitamin A stores. I wonder if spinach was the USA wartime equivalent of the UK carrot propaganda? How ironic that would be!
Why are these stories essential to debunk? Wikipedia states that during the first world war spinach was given to soldiers who had suffered haemorrhage, presumably to ‘replace’ iron. It was delivered in red wine – presumably to ‘help’ absorption, by chemical conversion to increase the solubility, by the acidity of the red wine. Red wine also contains iron – but also contains polyphenols, which will also inhibit the absorption of iron – likely a double error occurred in this case, then. Another point to make here is that diet alone currently cannot be used to treat anaemia. Usually, iron sulphate supplements are the chosen option, containing 65mg per dose, (which can, by the way, have devastating effects on digestive symptoms for those with IBS. Sodium federate is perhaps a better choice and if you have low iron/anaemia and IBS ensure your doctor has investigated the cause.) Although less of a ‘tonic’ than it was supposed to be, a ration of wine during World War 1 was probably welcomed by the soldiers.
What does this have to do with IBS you might ask? Well actually, rather a lot, particularly for those people who are vegans. The Low FODMAP diet is low in iron as many foods such as pulses and dried fruit – good sources of iron for vegans are limited on the diet. This shows the importance of proper knowledge and the impact of following such a diet has on nutrition and health. The importance of seeing a registered dietitian cannot be underestimated. Other sources are watercress, kale and include allowed portions of pulses with a source of vitamin C – although to what degree the overall polyphenol content of the vegan diet might affect absorption is not established and unlikely to be so. Digestion is complicated, this is a fact.
Spinach does have some really great other nutritional benefits, but it is no more a superfood concerning vitamin A content than the cheaply available carrot, (spinach has marginally more vitamin A content) or a good source of iron. It is, however, a source of vitamin K that can prevent blood clotting problems. The recipe below can be made for those who respond to a low fodmap diet and others who are just interested in tasty recipes!

Cream of spinach soup
- 100g Broccoli tops
- 35g carrots
- 70g celeriac
- 200g spinach (fresh or frozen)
- 1/4 teaspoon nutmeg
- 1/4 teaspoon cumin
- 1/4 teaspoon cinnamon
- 2 tablespoons of lactose-free mascarpone cheese
- 600ml water

Method
- Chop the vegetables finely
- Add them to a pan with 600ml water and spices
- Cook till soft
- Blend with a hand blender
- Add the mascarpone cheese just prior to serving
- Serves 4
https://www5.in.tum.de/~huckle/Sutton_Spinach_Iron_and_Popeye_March_2010.pdf
- Neveu V, Perez-Jiménez J, Vos F, Crespy V, du Chaffaut L, Mennen L, Knox C, Eisner R, Cruz J, Wishart D, Scalbert A. (2010) Phenol-Explorer: an online comprehensive database on polyphenol contents in foods. Database, doi: 10.1093/database/bap024. Full text (free access)
- Rothwell JA, Urpi-Sarda M, Boto-Ordoñez M, Knox C, Llorach R, Eisner R, Cruz J, Neveu V, Wishart D, Manach C, Andres-Lacueva C, Scalbert A. (2012) Phenol-Explorer 2.0: a major update of the Phenol-Explorer database integrating data on polyphenol metabolism and pharmacokinetics in humans and experimental animals. Database, doi: 10.1093/database/bas031. Full text (free access)
- Rothwell JA, Pérez-Jiménez J, Neveu V, Medina-Ramon A, M’Hiri N, Garcia Lobato P, Manach C, Knox K, Eisner R, Wishart D, Scalbert A. (2013) Phenol-Explorer 3.0: a major update of the Phenol-Explorer database to incorporate data on the effects of food processing on polyphenol content. Database, 10.1093/database/bat070. Full text (free access)